Simpler, Faster, Better Abscess Care
Quickloop®
Abscess Treatment Device



Simpler, Faster, Better Abscess Care
Quickloop®
Abscess Treatment Device


Why should you adopt the Loop Technique?
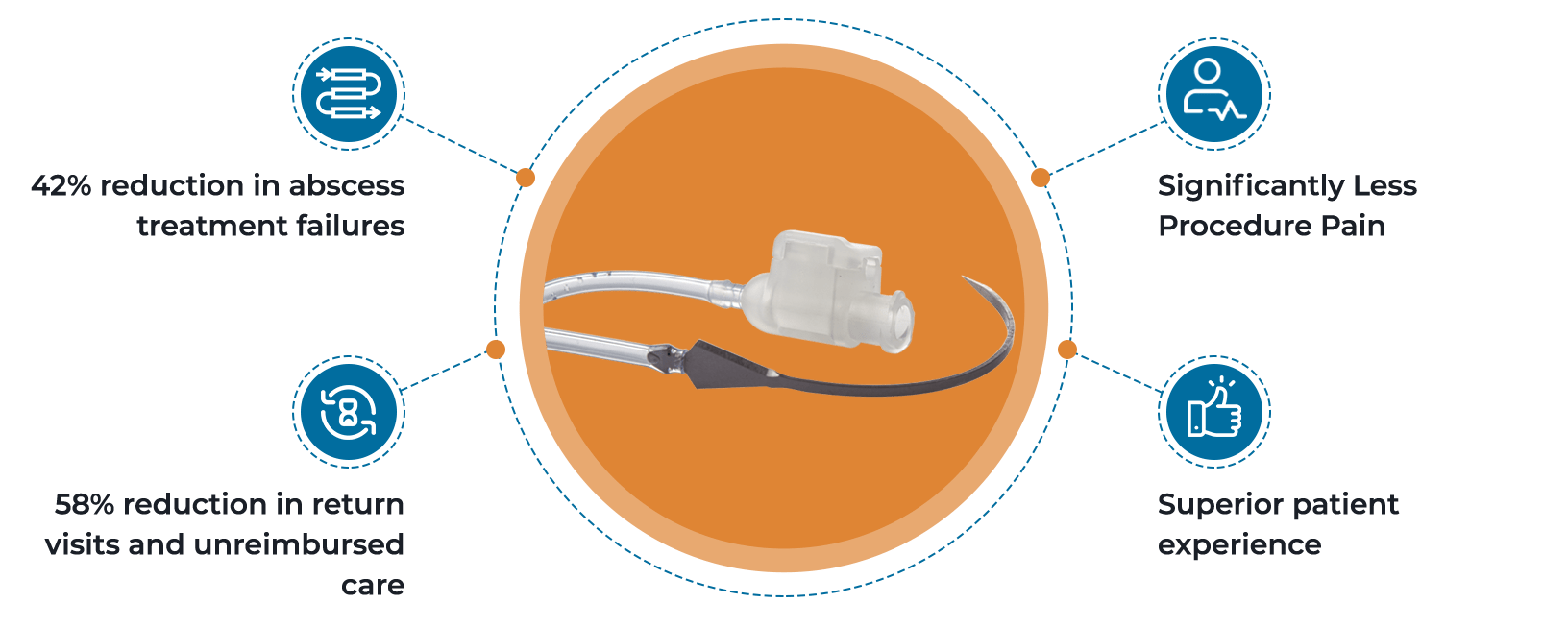
Loop Technique compared to traditional Incision and Drainage:
42% Reduction in treatment failures
58% Reduction in return visits
Significantly lower pain scores and easier home care
Significantly higher patient satisfaction
Benefits for Clinicans

42% Reduction in Abscess Treatment Failures
58% Reduction in return visits and unreimbursed care
Siginificantly Less Procedure Pain
Superior Patient Experience
Information for Patients
Your doctor usually has two ways they can treat your abscess. The older way is called Incision and Drainage (I&D). The newer way is with the Quickloop. The Quickloop way was made so you would have:
A shorter procedure
Less pain
A smaller scar
Fewer return visits to your doctor
Easier home care

Recent News
Dr. Mark Rosenberg Joins EM Device Lab Board of Advisors
Past President of the American College of Emergency Physicians (ACEP) will provide extensive clinical, business and leadership expertise.
...
Read MoreEM Device Lab Announces US Launch of the Quickloop® Abscess Treatment Device
An Advancement in Abscess Treatment that benefits clinicians, patients, and healthcare systems
...
Read MoreComprehensive Analysis Supports Loop Technique as Gold Standard for Abscess Treatment
EM Device Lab's Quickloop™ Abscess Treatment Device well-positioned for market entry
...
Read More